|
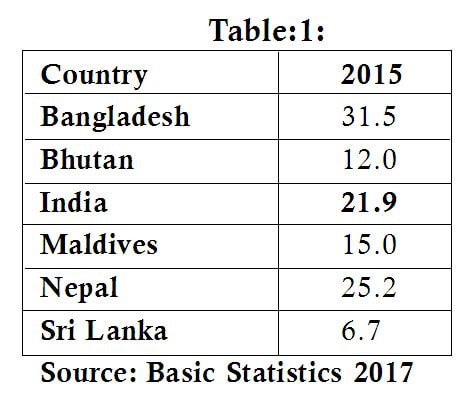
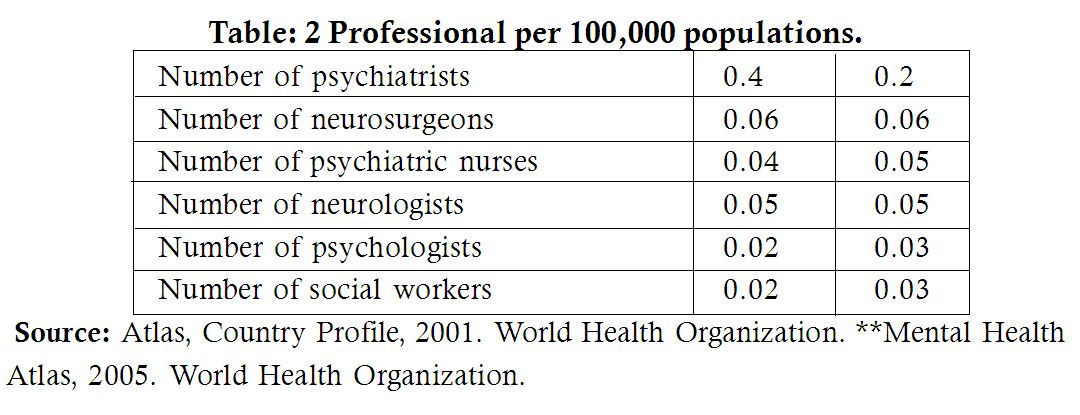
Introduction Managing good health is difficult due to many stressors in our daily life. A person with good in financial condition faces health problems and gets disturb psychologically sometimes. It is very challenging to have good health for people facing poverty because they face many stressors in day to day life. As we know, poverty is one of social problems in India. Poverty leads to other problems also. Poverty is an inability to fulfil the physiological needs, that is, need for existence, safety and security. The number of poor people in India, according to the country’s Eleventh National Development Plan, amounts to more than 300 million. The country has successful in reducing the proportion of poor people from about 55 percent in 1973 to about 27 percent in 2004, but almost one-third of the country’s of more than 11 billion continues to live below the poverty like, and a large proportion of poor people live in rural areas (R.Ahuja, 2014). Poverty definitions have been used differently by different authors and institutions. Common to most definitions is an idea of lack of resources as the cause or the condition of inability to meet minimum standards of living (Bennett 2006). Sociologist offers two definitions of poverty, absolute and relative poverty. Absolute poverty refers to lack of basic necessities such as food, shelter and income. Relative poverty refers to a situation in which some people fail to achieve the average income or lifestyle enjoyed by the rest of the society (M.U. Quareshi, 2004). There are many causes for poverty in India. Some important causes like rapidly rising population, low productivity in agriculture, under-utilised resources, low rate of economic development, price rise, unemployment, social factors, political factors and other factors. There are two extreme perspectives on the basis of which we can analyse the causes of poverty- the old and the modern. One view of poverty is that it is providential and it is the result of an individual’s past karma’s (deeds) or sins. The other view ascribes poverty to be the result of a failure of an individual’s working abilities or due to his/her lack of motivation. Financial condition is important to maintain good health status for every individual. Poverty also exposes people to risk factors for developing or worsening psychiatric disorders (R.Ahuja, 2014). Methodology: The study followed web based literature survey (secondary data) using Pubmed, Ebsco, Psyinfo, Government websites, etc by using key words such as poverty, causes of poverty, role of social worker in poverty. The researcher found on various aspects of poverty in India. The reviewer had chosen important studies for the review purpose. Results: In this review different aspects associated with mental health and poverty have been found. It is mentioned below: Relationship between Poverty and Mental Health: The relationship between poor mental health and the experience of poverty and deprivation has been well studied and an association between the two factors has been established (Kuruvilla & Jacob, 2007). Lund, Breen et all conducted a systematic review of the epidemiological literature in Low and Middle Income Countries (LMIC), with the aim of examining relationship between poverty and common mental disorders. Of 115 studies that were reviewed, most reported positive associations between a range of poverty indicators and CMD (Lund et al., 2010). Poor mental health linked to severe mental disorders has been associated with poverty during the recent economic crisis in middle-income and low-income countries, particularly India and China (Chatterjee, 2009; Kuruvilla & Jacob, 2007; Li, Pang, Du, Chen, & Zheng, 2012). The poor suffer worse health and die younger. They have higher than average child and maternal mortality, higher levels of disease, more limited access to health care and social protection, and gender inequality disadvantages further the health of poor women and girls. For poor people especially, health is also a crucially important economic asset. Their livelihoods depend on it. When a poor or socially vulnerable person becomes ill or injured, the entire household can become trapped in a downward spiral of lost income and high health care costs (OECD, 2003) Risk Factors: Different factors contribute to have mental health. Social, economic and physical environments impact on health status of person in any society. Risk factors for many common mental disorders are heavily associated with social inequalities, whereby the greater the inequality the higher the inequality in risk (Allen, Balfour, Bell, & Marmot, 2014). Poverty is easily understood as an individual -level risk factor, an ecological perspective on suicide that analyses the problem at a community level also suggests that areas of poverty, deprivation, unemployment and poor education are associated with higher suicide rates (Whitley, Gunnell, Dorling, & Smith, 1999). Poverty and Psychiatric Disorders: Poverty and associated conditions of unemployment, low educational level, deprivation and homelessness are not only widespread in poor countries, but also affect a sizeable minority of rich countries. Data from cross-national surveys in Brazil, Chile, India and Zimbabwe show that common mental disorders are about twice as frequent among the poor as among the rich (Patel, Araya, de Lima, Ludermir, & Todd, 1999). Poverty and suicide: Suicide is a multifactorial event. Suicide states to an act by which person desires to be dead, intents to die, and weather directly or through the actions of another person, he or she acts to achieve own death. (Fairbairn and Gavin 1995). While mental illness is a significant risk factor, researchers in developing countries including India, note that often it is the individual’s psychosocial context and stress which are the most common correlates of suicide. Among the commonly reported stressors are financial hardship, lower education and unfulfilled expectations at work (Manorantjtham, Abraham, & Jacob, 2005; Prasad et al., 2006). Suicides in India have been rising steadily over the last couple of decades. The number of suicides committed on economic grounds has more than doubled between 1991 and 2009 (P. Amitendu and Amitendu, 2011). Poverty combined with indebtedness has most distressing effects reflected in suicides in South Asia. In India also during the period of 5 years from 1998 to 2003, official figures show that more than 100,000 small farmers have committed suicide (Upadhyaya 2008). Mental health issues associated with poverty: The relationship between poverty and mental health can be explored under various headings. The economic burden for psychiatric disorders: The existence of mental health problems results in huge financial burden on individuals, their families and society as a whole. Pain as a result of poverty: Poverty brings along with it a lack of opportunity, reduced availability and accessibility to resources and a greater likelihood of experiencing difficult events. The resultant distress may manifest in a variety of presentations including emotional states such as low mood and sadness, frustration or discontent; in the Indian setting many individuals may also present with physical symptoms for which there is no identifiable organic cause. On enquiry the individual often attributes his problems to the state of poverty and its attendant hardships (Kuruvilla & Jacob, 2007). Mental Health, Poverty and Children: Research suggests that household income influences child mental health. Children from low income families appear to have higher levels of depression and anti-social behaviour -such as bullying, being cruel, breaking things, cheating or telling lies than children from more advantaged households. Children in chronically poor families show lower cognitive performance. A change in household income also influences the child’s mental health. Drops in income increase depression and anti-social behaviour, while a move out of poverty and an improvement in household income results in improved child mental health (Strohschein, 2005). Shame and Poverty: Amartya Sen has reiterated that shame is a universal attribute associated with poverty. Shame is commonly accompanied by the fear of being humiliated, ridiculed or laughed at, consequential to the exposure, real or imaginary, of one’s weaknesses, failure, evil, in front of others. One feels vulnerable, stripped of one’s persona. (Fai Ho, Fu og Ng 2004). Poverty as a risk factor for psychiatric illness: People with poor financial condition face stressors when they do not have opportunities to fulfil their basic needs. Poor people face financial hardships which cause stressors in their life. These stressors can lead to Depressive disorder among such people. The one of the study shows that association between economic factors and psychiatric illness. The study conducted by Patel & Kleinman, it shows that Poverty, acting through economic stressors such as unemployment and lack of affordable housing, is more likely to lead psychiatric illnesses such as depression and anxiety, hence making it an important risk factor for psychiatric illness (Patel & Kleinman, 2003) Women, poverty and mental health: Being female is reported to be a risk factor for common mental disorders. Studies from India have shown that poverty and deprivation are independently associated with the risk for common mental disorder in women and add to the sources of stress associated with womanhood (Patel, Kirkwood, Pednekar, Weiss, & Mabey, 2006). Mental health was a much neglected field until recently. There is, however, increasing realization that conditions such as schizophrenia, mood disorders (bipolar, manic, depressive and persistent mood disorders) and mental retardation can impose a marked disease burden on Indians. This was confirmed by a study conducted for the National Commission on Macroeconomics and Health (NCMH) which stated that at least 6.5% of the Indian population had some form of serious mental disorder, with no discernible rural–urban differences; women had slightly higher rates of mental disorder than men (NCMH, 2005). Poverty, Non-compliance issues and Relapse of Psychiatric illness: Compliance (also adherence, concordance) describes the degree to which a patient correctly follows medical advice. It is important to note that the term compliance applies not only to pharmacological treatment but also to all kinds of other measures involved in treatment, such as socio therapeutic and psychotherapeutic interventions. There are various factors contribute to noncompliance among psychiatric patients e.g. lack of insight towards psychiatric illness, financial problems, drug related factors, interpersonal factors, religious beliefs, social support, doctor-patient relationship, time taken to improve and long distance where patient has to come to psychiatric hospital for taking treatment, family member’s pressure etc. Noncompliance issues lead to relapse of psychiatric illness. Poor people suffering from severe psychiatric disorders cannot afford long term psychiatric drugs. They discontinue medication in treatment process due to financial problems. Person suffering from Schizophrenia is a severe psychiatric disorder and having below poverty level income which may lead to noncompliance issues in treatment process. It is important to understand that people facing poverty are often incapable to afford treatment or have to spend high amounts of their profits on treatment. People living in poverty face difficulties to pay the amount on treatment at even private hospitals. Share population below the National Poverty Line: The below table indicates share of population below the National poverty line Shortage of Mental health professionals: There is a dearth of mental health professional to provide adequate mental health services for huge population like India, China and in other counties. And there is shortage of mental health professionals in Government sectors and steps have been taking to increase number of steps to provide quality of services at Government level. The following table shows mental health professionals per one lakh population. Discussion: Health is “a state of complete physical, social, and mental well-being and not merely the absence of disease or infirmity” (WHO, 2006). Yet, our health system is pre-occupied with curative health care amenities and disease prevention, with slight consideration on social and mental wellbeing. Among these, mental health and well being is the most ignored one (Kumar, A. 2001; & Kumar, A., 2010) particularly in rural areas (Thara, R., Padmavati, R. and Srinivasan, T. 2004; Meltzer, M. 2008). It shows that we need to give more importance to mental health, especially poor people living in our country. It is estimated that 6-7 % of population suffers from psychiatric disorders. In the world, about 450 million people were estimated to be suffering from neuro-psychiatric conditions. These conditions included unipolar depressive disorders, bipolar affective disorder, schizophrenia, epilepsy, alcohol and selected drug use disorders, Alzheimer’s and other dementias, post-traumatic stress disorder, obsessive and compulsive disorder, panic disorder, and primary insomnia. Most strongly associated factors with mental disorders are deprivation and poverty. Individuals with lower levels of education, low household income, lack of access to basic amenities are at high risk of mental disorder (Patel V, Kirkwood BR, Pednekar S, Weiss H, Mabey D, 2006). 72.2 per- cent of population lives in rural areas, with only about 25 percent of the health infrastructure, medical man- power and other health resources, it may be surmised that the number of people affected with any mental and behavioural disorder would be higher in rural areas (Gururaj, G., Girish, N. and Isaac, M.K. (2005). People living in rural areas not able to get immediate mental health care services compare to urban population. There is a shortage of psychiatric facilities in the in rural areas. National Mental Health Program (NMHP) has been mental implemented in 1982. The main objectives of the NMHP are to ensure the availability and accessibility of minimum mental healthcare for all in the foreseeable future, particularly to the most vulnerable and underprivileged sections of the population, to encourage the application of mental health knowledge in general healthcare and in social development; and to promote community participation in the mental health service development and to stimulate efforts towards self-help in the community. The study by Narayan D et al. in 2000 show that mental health problems are often raised jointly with physical concerns, and hardships associated with drug and alcohol abuse are also frequently discussed. Stress, anxiety, depression, lack of self-esteem and suicide are among the effects of poverty and ill-health commonly identified by discussion groups Narayan D et al. (2000). It is interesting to note that the poverty of a country does not necessarily mean that mentally ill people will receive poor care. Experiences in some African, Asian and Latin American countries show that adequate training of primary health care workers in the early recognition and management of mental disorders can reduce institutionalization and improve clients’ mental health (WHO, 2001). National Mental Health Program and District Mental Health Program have been providing mental health services and training medical officers, health workers and staff of different organizations to identify mental health problems. Though, people living in below poverty line approach faith healers at their nearest places due to stigma of mental illness or financial issues. The World Health Report lists the key determinants of mental health to be poverty (and its associated conditions of unemployment, low educational attainment, deprivation, homelessness), gender, age, conflicts and disasters, major physical diseases, family and environmental factors (WHO 2001). When we look at meaning of mental health, it is a state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and is able to make a contribution to his or her community. How can people with below poverty line can able to lead life without coping with stressors to fulfil their basic needs, is highly challenging.
The study by Trani J-F, Bakhshi P, Kuhlberg J, et al in in 2015, provides evidence that mental health professionals must incorporate an understanding of multidimensional poverty stressors as well as address family and community dynamics. The role of social worker in mental health is to educate patients having poverty, issuing them disability certificates if they meet disability criteria as per Indian Disability Evaluation and Assessment Scale (IDEAS) to access social welfare benefits. Social worker need to provide information about psychiatric facilities at patient’s nearest places, so they can save the money by approaching nearest psychiatrist. Addressing non-compliance issues to psychiatric patients could prevent relapse of psychiatric illness. Conclusion: Mental health services need to be provided for poor people having psychiatric problems without any charges. Government has been investing huge effort to develop manpower in the field of mental health in our country. But, it takes time to have required mental health professionals. Social work professionals working in the field of mental health need to explore different psychosocial problems of poor people who seek counselling and treatment at psychiatric hospitals or psychiatric nursing homes. Effective psychosocial interventions can be given for such patients. Reference:
Ashok S.Kori Psychiatric Social Worker, Dharwad Institute of Mental Health and Neurosciences (DIMHANS), Dharwad. |
Categories
All
Social Work Learning Academy50,000 HR PROFESSIONALS ARE CONNECTED THROUGH OUR NIRATHANKA HR GROUPS.
YOU CAN ALSO JOIN AND PARTICIPATE IN OUR GROUP DISCUSSIONS. MHR LEARNING ACADEMYGet it on Google Play store
|
SITE MAP
SiteTRAININGJOB |
HR SERVICESOTHER SERVICESnIRATHANKA CITIZENS CONNECT |
NIRATHANKAPOSHOUR OTHER WEBSITESSubscribe |
MHR LEARNING ACADEMY
50,000 HR AND SOCIAL WORK PROFESSIONALS ARE CONNECTED THROUGH OUR NIRATHANKA HR GROUPS.
YOU CAN ALSO JOIN AND PARTICIPATE IN OUR GROUP DISCUSSIONS.
YOU CAN ALSO JOIN AND PARTICIPATE IN OUR GROUP DISCUSSIONS.
|
|





 RSS Feed
RSS Feed





