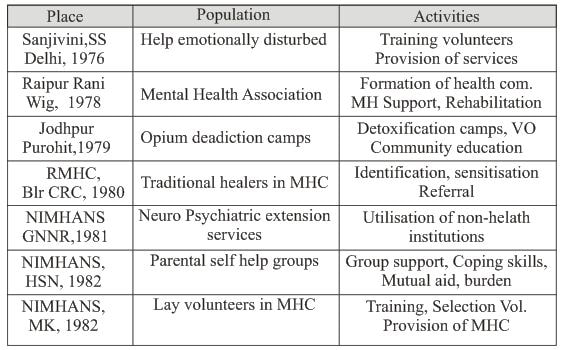
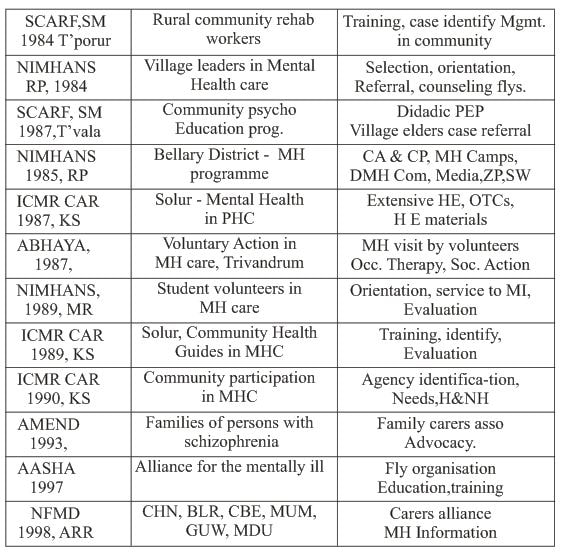
Community inclusion for people with psychiatric disabilities and role of Psychiatric Social Worker1/1/2018 Introduction In many countries of the world today, people with disabilities are deprived of their rights and liberties, excluded from society, and blamed for many of society's most unsolvable problems, such as crime and homelessness. People with disabilities, particularly people with mental disabilities are involuntarily locked away in institutions, subjected to abuse and neglect, and deprived of their right to live as equal citizens in the community. Persons with disabilities often are excluded from the mainstream of the society and denied of their human rights. Studies now suggest that treatment through community inclusion for many people with mental disabilities in the world is less costly than institutionalization, and that treatment is usually more effective.(1) Unnecessary confinement diminishes the individual's ability to have a social life and family relations, to receive an education, or to become economically independent through employment. Thus, undue institutionalization is discriminatory not only because it treats people with and without disabilities differently in terms of their access to mental health treatment, but also because it perpetuates negative stereotypes of people with mental disabilities as "incapable or unworthy of participating in community life," and deprives them of "everyday life activities" such as "family relations, social contacts, work options, economic independence, educational advancement, and cultural enrichment Definition of psychiatry disability The Americans with Disabilities Act (ADA) defines disability as a physical or mental impairment that substantially limits a major life activity; a record of such an impairment; or being regarded as having such an impairment. Impairments: include major depression, bipolar disorder, anxiety disorders, obsessive compulsive disorder, post-traumatic stress disorder, schizophrenia, and personality disorders, but not traits or behaviors like irritability, chronic lateness or poor judgment. Major Life Activities: are learning, thinking, concentrating, interacting with other sand sleeping. Substantial Limitation: means a person with a disability cannot perform a major life activity the way the average person in the general population can perform the same activity. Who Determines the Disability? Expert testimony is not required to prove substantial limitation. Credible testimony from the person with the disability, family, friends, or co-workers may be enough. What about Medication? Use of medication should not be considered when deciding whether impairment is substantially limiting. How Long? An impairment that lasts for more than several months and significantly restricts a major life activity is substantially limiting. Does it have to be continuous? No. Chronic, episodic conditions can be substantially limiting when they are active or have a high chance of recurrence in substantially limiting forms.(2) Another definition of psychiatric disability is Persons who suffer from certain mental or emotional disorders that prevent the development of their functional capacities in relation to primary aspect such as personal hygiene and self care, self-direction Inter-personal relationships, social interaction learning and recreation. (Goldman et al., 1981) Prevalence of Psychiatry Disability- 450 million people suffer from mental or behavioral disorder. Neuro psychiatric disorders account for nearly one third of the disability in the world. Severe mental disorders figure among the 10th leading causes of disability and burden to the world (3) Releasing the report, WHO Regional Director for South East Asia Regional Uton Muchtar Rafei said that in the South East Asian region 27 per cent or nearly one third of disability is due to neuropsychiatric disorders. The mortality statistics, however, does not reflect the burden of mental and neurological disorders, which cause untold sufferings In India over 125 million people suffer from Mental Illness. Prevalence rates have increased due to poverty, illiteracy, urbanization, industrialization, discrimination, better diagnostic methods and increased public awareness. Estimated population of chronic psychotic patients in India will be 50 millions by 2010.(4) The Impact of Mental Illness on Community Mental and behavioural disorders have a large impact on individuals, families and communities. Individuals suffer from the distressing symptoms of disorders. They also suffer because they are unable to participate in work and leisure activities, often as a result of discrimination. They worry about not being able to shoulder their responsibilities towards family and friends, and are fearful of being a burden on for others. It is estimated that one in four families has at least one member currently suffering from a mental or behavioural disorder. These families are required not only to provide physical and emotional support, but also to bear the negative impact of stigma and discrimination present in all parts of the world. While the burden of caring for a family member with a mental or behavioural disorder has not been adequately studied, the available evidence suggests that it is indeed substantial (Pai & Kapur 1982; Fadden et al. 1987; Winefield & Harvey 1994). The burden on families ranges from economic difficulties to emotional reactions to the illness, the stress of coping with disturbed behaviour, the disruption of household routine and the restriction of social activities (WHO 1997a,) The impact of mental disorders on communities is large and manifold. There is the cost of providing care, the loss of productivity, and some legal problems including violence associated with some mental disorders, though violence is caused much more often by “normal” people than by individuals with mental disorders. (3) The Global Burden of Disease study developed a single measure to allow comparison of the burden of disease across many different disease conditions by including both death and disability. This measure was called Disability Adjusted Life Years (DALYs). DALYs measure lost years of healthy life regardless of whether the years were lost to premature death or disability. The disability component of this measure is weighted for severity of the disability. For example, disability caused by major depression was found to be equivalent to blindness or paraplegia whereas active psychosis seen in schizophrenia produces disability equal to quadriplegia. Using the DALYs measure, major depression ranked second only to ischaemic heart disease in magnitude of disease burden in established market economies. Schizophrenia, bipolar disorder, obsessive-compulsive disorder, panic disorder, and post-traumatic stress disorder also contributed significantly to the total burden of illness attributable to mental disorders. The projections show that with the aging of the world population and the conquest of infectious diseases, psychiatric and neurological conditions could increase their share of the total global disease burden by almost half, from 10.5 per cent of the total burden to almost 15 per cent in 2020.(5) Meaning of Community inclusion: Inclusion means that people with mental illness are recognized as individuals with the right to take risks, to make choices, to make mistakes, to be independent and to reap the benefits of physical activity in the same way as any other person in the Community (Captivate, 2008) We have to adapt their structures and procedures to facilitate the inclusion of people with psychiatric disabilities, rather than expecting them to change to fit in with existing arrangements. It places the focus on all citizens and their entitlement to equal treatment, again reinforcing the fact that the rights of all people, including those with disabilities, must be respected. The community looks at itself and considers how policies, laws, and common practices affect all community members (6) Barriers to Community Inclusion: Just like wheelchairs and Braille have increased social integration for people with physical handicaps, there is also a need to identify and remove the barriers to community inclusion for people with serious mental illness," says Prof. Roe. Some of the barriers are; direct manifestations of psychopathology, names of illnesses are themselves a barrier, Interference in functional capabilities in daily life such as Self Care, Communication, Interpersonal Relationships and Work, Learning and applying knowledge, General tasks and demands, Mobility, Major life areas, social and civic life, and cultural life. (7) Stigma is defined as a sign of disgrace or discredit, which sets a person apart from others. Stigma is a term used to describe a process where a person is denied full and equal social standing with another person, another obstacle that may result from stigma is "self-stigma”. Whereby people with a mental illness adopt and internalize the social stigma and experience loss of self-esteem and self efficacy. "People with a mental illness with elevated self-stigma report low self-esteem and low self-image, and as a result they refrain from taking an active role in various areas of life, such as employment, housing and social life. In a survey of discrimination faced by people who experienced mental health problems,47% had been verbally or physically harassed in public because of their mental health problems. 14% had been physically attacked and 26% of men and 48% of women believed their parenting abilities had been unfairly questioned(8) Community inclusion through respecting human rights and legislation : Mental health policies and programmes should promote the following rights: equality and non-discrimination; the right to privacy; individual autonomy; physical integrity; the right to information and participation; and freedom of religion, assembly and movement. Human rights instruments also demand that any planning or development of mental health policies or programmes should involve vulnerable groups (such as indigenous and tribal populations; national, ethnic, religious and linguistic minorities; migrant workers; refugees and stateless persons; children and adolescents; and elderly people) in the planning and development of mental health policies and programmes. Beyond the legally binding International Covenant on Civil and Political Rights and the International Covenant on Economic, Social and Cultural Rights, which are applicable to the human rights of those suffering from mental and behavioural disorders, the most significant and serious international effort to protect the rights of the mentally ill is the United Nations General Assembly Resolution 46/119 on the Protection of Persons with Mental Illness and the Improvement of Mental Health Care, adopted in 1991 (UN 1991). Although not legally binding, the resolution brings together a set of basic rights which the international community regards as inviolable either in the community or when mentally ill persons receive treatment from the health care system. There are 25 principles which fall into two general categories: civil rights and procedures, and access to and quality of care. Principles include statements of the fundamental freedoms and basic rights of mentally ill persons, criteria for the determination of mental illness, protection of confidentiality, standards of care and treatment including involuntary admission and consent to treatment, rights of mentally ill persons in mental health facilities, provision of resources for mental health facilities, provision of review mechanisms, providing for protection of the rights of mentally ill offenders, and procedural safeguards to protect the rights of mentally ill persons. The United Nations Convention on the Rights of the Child (1989) provides guidance for policy development specifically relevant to children and adolescents. It covers protection from all forms of physical and mental abuse; non-discrimination; the right to life, survival and development; the best interests of the child; and respect for the views of the child. There are also a number of regional instruments to protect the rights of the mentally ill, including the European Convention for Protection of Human Rights and Fundamental Freedoms, backed by the European Court of Human Rights; Recommendation 1235 (1994) on Psychiatry and Human Rights adopted by the Parliamentary Assembly of the Council of Europe; the American Convention on Human Rights, 1978; and the Declaration of Caracas adopted by the Regional Conference on Restructuring Psychiatric care in Latin America in 1990. The human rights treaty monitoring bodies represent one example of an underutilized means to enhance the accountability of governments as regards mental health and to shape international law to address mental health matters. Nongovernmental organizations and the medical and public health professions should be encouraged to make use of these existing mechanisms to prompt governments to provide the resources to fulfill their obligations towards the health care of persons with mental disorders, protecting them from discrimination in society, and safeguarding other relevant human rights.(3) India: NMHP 1982: One of the objectives of NMHP is to promote community participation in the mental health service development and to stimulate efforts towards self help in the community and its Specific approach is Integration of basic mental health care in to general health services Linkage to community development (9) China -Article 3 of the Law sets a principle of anti-discrimination that stipulates; “Disabled persons are entitled to enjoyment of equal rights as other citizens in political, economic, cultural and social fields, in family life and other aspects (10) Community inclusion programmes in India and other countries: Israel The development of many new projects by the consumers and self-advocates were also a major factor in supporting and encouraging professional and family members to promote the inclusion of persons with psychiatric disabilities in the community. Since 1997. There has been an increase in the work of self-help organizations, such as "BENAFSHENU" that was jointly initiated by consumers and service workers. This is a unique service, as the BENAFSHENU staffs are people coping with mental illness. Their personal experience instills trust and mutual understanding, enabling them to act as mediators between the consumers and the establishment, to promote the consumer population's quality of life (11) Another project is "LAHAK," which promotes leadership development among the population with psychiatric disabilities, who then serve as role models for their members. Participation in this kind of project opens up opportunities to take part in many developing projects, such as "Voices", a website established in 1997,the Internet has become a powerful vehicle for empowerment and accessibility to the media, enabling interaction between people, especially for those who have difficulty leaving the house It provides them with a platform where they can express themselves through art, poetry, literature and academic writing and can also receive counseling and practical information via the website The impact of self-help organizations has increased hopes and beliefs, and professionals and consumers are now running various types of joint training programs, with mutual recognition of the special impact of each group (Lachman, 1998; Rivlin, 2002). (12) Peru – community programmes 1. Establish human rights oversight and monitoring for mental health services, both in institutions and in the community. A. Developing independent oversight and accountability to monitor compliance with national legislation and international human rights principles for persons with mental disabilities, including a system to investigate allegations of abuse that would protect the privacy and safety of victims and witnesses. B. Create a complaint mechanism, whereby people with disabilities can report abuse in mental health services without fear of reprisals. 2. Ensure the inclusion of stakeholders in the planning and implementation of medical, mental health, and social services for people with mental disabilities. A. Reform article 6 of Law 27050, regarding the composition of the National Council for the Integration of Persons with Disability (CONADIS), to include representation of persons with psychiatric disabilities. B. Funding stakeholder advocacy so that people with mental disabilities and family members have the resources necessary to fully participate in the planning and policy-making process, particularly regarding policies that concern them. Community-inclusion models: Group home: The home has a family environment in which attention is given to the residents’ needs for individual development, recreational activities, privacy, and personal space. At the home, investigators observe a well-trained, caring, and dedicated staff engaged in facilitative activities with residents, one of whom has a job at an integrated workplace in the community. Promising model This model proposes working in community itself and students with severe mental retardation, autism, and emotional and behavioral difficulties, and their families. The theory behind the Center is to train parents and family members to work with their children. Families should attend 90 hours of parent education annually, ensuring that the instruction provided in the Center’s setting is reinforced at home. The model also provides a continuing education and service program for students and their families throughout the student’s life, and helps place students in community-integrated jobs (13) Community inclusion programmes in India: Social support system: Social support most commonly refers to helpful functions performed for an individual by significant others such as family members, friends, co-workers, relatives and neighbors. Social support in India plays vital role while rehabilitating the psychiatric disabilities (14) “There is much that United States and Europe could learn from villages in India” “Social factors play a major and important role in the outcome of disease” Very few solutions are medical in medicine”, says Norman Sartorius, Former head of WHO’s mental health programme Religious organizations: Mental health professionals have to link with the Temples Faith healers, Traditional Healers, Sooth Sayers, Seers and sages, Palm readers, Churches, Masques. If they get any mental ill patient they can him refer to mental health services and also while person the disabilities in the community all religious leaders should educate the community, With out affecting their occupation government and NGOs have to come forward to mediate between the religious leaders and mental health professionals (15) Inclusion through family care: The family and the community in India have always played a significant role in the management of the chronic mentally ill in the community (16,) Research findings show that better outcomes are achieved for people with mental illness by involving and working with their family carers in an educational and supportive partnership.Prof. Ian Falloon. Support groups ( self help groups) Among the psychiatric patients and their family members of them support groups or self help groups can be started To Identify relapse triggers and strengthen coping strategies To Initiate life skills development To Assist in recognizing negative emotions and in dealing with them appropriately To Facilitate involvement in healthy recreational activities To strengthen family and other social support. Community inclusion through NGOs: NGOs are recognized by Government as non profit or welfare oriented organizations and Play a key role as advocates, service providers, activists and researchers on a range of issues pertaining to mental health services. Especially NGOs are working in community itself with various programmes in all levels of psychiatric disabilities inclusion. (17) Awareness programmes: Strengthening community awareness about the complexities of mental illness and reducing its associated stigma, enabling psychiatric patients lead a normal life in community itself is the aim of mental health awareness programmes.People who may be experiencing mental health symptoms seek appropriate help and with increased knowledge their family, friends and carers recognise their own needs for support.” School teachers,Anganwadi Workers, Gramapnchayath members , village leaders , voluntary workers can spread awareness through Media, TV, Radio,Pamplets, Brochers, Streeat play and Drama. (18, 19) Culture, Sports and Recreation: Public cultural facilities, such as libraries, museums, art galleries, public parks, and sports venues are open to and expected to make reasonable accommodations for people with disabilities. Depending on the policies of local authorities, admittance to such activities may be available free of charge. Community inclusion through educational institutions: Inclusive and appropriate education for children with intellectual disabilities. Integrating children with mental disabilities in mainstream classrooms will require training for teachers, and teachers’ aides may be necessary in some classrooms. Indian educational system should also provide programs in speech pathology, physical therapy, and mental health services to enable children with disabilities to benefit from an education. Schools, Colleges, Technical Institutes, Professional Course institutions, non – formal educational institutions, and Special institutions should have subject on mental health and should encourage the student with psychiatric illness students for continuing their education. Vocational training in community: Vocational training services prepare qualified applicants to achieve a lifestyle of independence and integration within their workplace, family and local community. This transition is achieved through work evaluation and job readiness services, job counseling services, and medical and therapeutic services. For individuals with psychiatric disabilities, situational assessments are generally used to evaluate vocational skills and potential. In the community vocational training can be given. Through that, psychiatric disabled can earn money, which helps him family as well as his treatment purpose. Once the patient is trained in particular work, with the help of government, NGos, private partnership, families, he can be placed. (20, 30) Empowering through participation in treatment planning: All levels of treatment plan, discharge and rehabilitation patients and their family members should be included by the treating team. It should be based on both psychological and organizational factors. For this patient needs a minimal level of psychiatric stability and decision-making skills as well as an organizational culture that promotes shared decision making and provides the resources required for empowerment.(21) Participation in treatment planning also can be empowering when people with mental illness choose their own goals and the treatment activities that best support the goals they have selected for themselves. Choice is now considered fundamental to the recovery process for this group (Bassman, 1997) Through liaisons: Communication and liaison between GPs, mental health professionals, Occupational health staff is an essential part of keeping people with psychiatric Disabilities in work or getting them back to work (22) Community based rehabilitation (CBR) It is a “Strategy within community development for the rehabilitation, equalization of opportunities, and social integration of all people with disabilities. CBR is implemented through the combined efforts of disabled people themselves, their families and communities. The appropriate health, education, vocational and social services are provided through the CBR).(23) Objectives of CBR: Working with and through the community To create positive attitudes towards people with disabilities. Meeting their needs and giving them equal opportunities. To develop their full potential To become full-fledged, contributing members of the society in a friendly environment Through media Media has a vital role to play in community inclusion of people with psychiatric disability. Hence media personnel should be educated on mental health issues.(24) Mental health insurance: Based on model of health insurance with a low premium, it should, include all types of psychiatric disabilities. Hospital expenses, medication and investigations should be covered in life insurance. Key features include: Immediate settlement of claims. Emergency loans on the base of insurance Network hospitals Helping hands in all steps ( 13,25) Mental Health Helpline The helpline can be established with the aim of rescuing wandering persons with mental illness and to avoid duplication of services by networking. The personnel managing police helpline also would provide mental health multidisciplinary services. This kind of service has been initiated by Karuna trust (13, 26) Telemedicine Services to PHC: Emergency mental health services and referral services can be given with the help of ISRO to all PHCs in the country and can connect the primary health care centers with leading mental health tertiary care centers for future follow-up services. (13, 27) Access psychiatric medication in community: Barriers to adequate community-integrated mental health services are also created by the government. The average cost of psychiatric medication is two times more than the basic monthly income a family member in rural India. So many patients would not come for follow up and for continue medication. The government can provide increased accessibility to psychotropic and other psychiatric medication with free of cost. Primary Health Care through Public-Private Partnerships (ppp): Primary Health Care is a work towards meeting people's basic health needs through a comprehensive, remarkably progressive approach and its includes promotion basic health needs, but considering the predominance of the rural population, great emphasis was placed on the development of infrastructure techniques and manpower for service delivery mainly in rural areas. The National Rural Health Mission (NRHM: 2005-2012) by the Government of India planned to set up PPPs at different levels of health care as key partners to success in implementation. So with private partnership psychiatric disabilities can be rehabilited at their communities through vocational training, providing work at community, providing emergency psychiatric health services, (28) Example;Integration of epilepsy &mental health Began in the Gumballi PHC in 1996 with support from NIMHANS Karuna Trust, Karnataka Community participates in mental health care (Indian experiments): Community participation is a process of activities comprising people’s involvement in decision making, contributing to the development efforts, shared equitably in the benefits derived there from. Community should be encouraged not only to identify and express the mental health needs of their people, but to seek ways by which these needs can be met from their local resources with minimal assistance. (29) All people in the community should actively involve to include the psychiatric disabled among them. Some of the experiments are; (31,32) Conclusion:
The psychiatric social worker will play a vital role in above all the community inclusion programmes for psychiatric disabilities. At the community level, the atmosphere could be changed by the systematic implementation of various mental health interventions directed at the modification of the local community's beliefs and attitudes towards the interactions of the mentally ill and it can be guided by only community mental health act or policy. (33) Reference 1) Eric Rosenthal and Arlene Kanter, The Right to Community Integration for People with Disabilities Under United States and International Law, http://www.dredf.org/international/paper_r-k.html. 2) Paula N. Rubin, Esq., The ADA and Psychiatric Disabilities:New Guidance from the EEOC. 3)WorldHealthOrganization.Worldhealth report2001—Mental health:New understanding, new hope, Geneva 4) UNI AJ MS , BK1906 , 4 October 2001, ZCZC, DI 68 ) 5) NIH Publication No. 99-4586 6) A Strategy for Rehabilitation,Equalization of Opportunities,Poverty Reduction and Social Inclusion of People with Disabilities, Joint Position Paper 2004 7) Prof. David Roe,New intervention to reduce self-stigma among persons with serious mental illness, Collaboration between researchers at the University of Haifa, City University of New York and Indiana University. 8) Jim Read & Sue Baker A, Survey of the Stigma, Taboos and Discrimination Experienced by People with Mental Health Problems, November 1996 The Mental Health Charity. 9) The National Mental Health Programme (NMHP),1982 10) Eric zhang guozhong,inclusion of persons with disabilities in China, asia pacific disability rehabilitation journal 11)http://www.benafshenu.jerusalem.muni.il 12) http://www.voices.co.il , 13) Lima, human rights & mental health in peru ,mental disability rights international& asociación pro derechos humanos September 2004 14) Sudipto Chatterjee, Evaluation of a community-based rehabilitation model for chronic schizophrenia in rural India, The British Journal of Psychiatry (2003) 182: 57-62 15) Daya Somasundaran, Mental health in the Tamil community, Transcultural psychosocial organization, Japna 16) Chandrasekhar CR, Parthasarathy R: Community Psychiatry. in Textbook of Post Graduate Psychiatry. 2nd edition. Edited by: Vyas JN, Ahuja N. New Delhi: Jaypee Brothers Medical Publishers; 1999:985-992. ) 17) Vikram Patel, R,Tara Meeting the mental health needs of developing countries: NGO innovations in India, 2003 18) Community Mental Health Programme Awareness Campaign,July 2009, the Banyan 19) Rangawsamy Thara , Ramachandran Padmavati* Jothy R Aynkran* and Sujit John, Community mental health in India: A rethink, International Journal of Mental Health Systems 2008 ) 20) Gary L. Fischler, Ph.D., and Nan Booth, M.S.W., M.P.H; Gaithersburg, Maryland, Aspen Publishers, 1999, 258 pages, Vocational Impact of Psychiatric Disorders: A Guide for Rehabilitation Professionals, 21) Linhorst, Donald M.; Hamilton, Gary; Young, Eric; Eckert, Anne, Opportunities and barriers to empowering people with severe mental Illness through participation in treatment planning, social work ,ctober 1, 2002 22) Leigh H, Multidisciplinary teams in consultation-liaison psychiatry: the Yale model, Psychother Psychosom. 1987;48(1-4):83-9 23) United Nation Agencies, ILO, UNESCO, WHO, 1994 24) Mark Salter, Psychiatry and the media: from pitfalls to possibilities, Psychiatric Bulletin (2003) 27: 123-125 25)ellakavi.wordpress.com/2007/10/22/karuna-trust/ 26)http://www.nibsindia.org/mentalhealthhelpline.html 27) Joseph Tracy, Telemedicine, Technical Assistance Documents,2004, 28) Pal R, Pal S. Primary health care and public-private partnership: An indian perspective. Ann Trop Med Public Health 2009;2:46-52 29) WHO TRS 564, 1975 30) Steven.p.Segal,The mental illness in community based sheltered care, A study of community care and social integration. 31) Agarwal S.P (1985), Mental Health: An Indian Perspective 32) Srinivasa Murthy, R. & Burns, B. (Eds.). 1987. Proceedings of the Indo- US symposium on community mental health. Bangalore: National Institute of Mental Health & Neuro Sciences ;37:405–419. Kannappa Shetty (M.phil scholar) Mr. Sanjeev Kumar (PhD scholar) Dr. B.P.Nirmala Assistant Professor, Dept. of PSW NIMHANS, Bengaluru-29 |
Categories
All
Social Work Learning Academy50,000 HR PROFESSIONALS ARE CONNECTED THROUGH OUR NIRATHANKA HR GROUPS.
YOU CAN ALSO JOIN AND PARTICIPATE IN OUR GROUP DISCUSSIONS. MHR LEARNING ACADEMYGet it on Google Play store
|
SITE MAP
SiteTRAININGJOB |
HR SERVICESOTHER SERVICESnIRATHANKA CITIZENS CONNECT |
NIRATHANKAPOSHOUR OTHER WEBSITESSubscribe |
MHR LEARNING ACADEMY
50,000 HR AND SOCIAL WORK PROFESSIONALS ARE CONNECTED THROUGH OUR NIRATHANKA HR GROUPS.
YOU CAN ALSO JOIN AND PARTICIPATE IN OUR GROUP DISCUSSIONS.
YOU CAN ALSO JOIN AND PARTICIPATE IN OUR GROUP DISCUSSIONS.
|
|





 RSS Feed
RSS Feed





