|
Abstract Alcohol addiction has been termed as a ‘family disease’. The impact of alcohol addiction on the families living with individual with addiction is enormous and has been documented. However the family and care takers who significantly contribute to the care, process of treatment, recovery and rehabilitation of the individual with alcohol addiction hardly receive any attention and intervention in the de-addiction process of the client. Families and their member living with individual with alcohol addiction can be termed as passive sufferers. The authors believe that strengths based practice that has an emphasis on positive qualities and attributes, is quite likely to produce a different approach to social work practice with the families with alcoholic as well as clients that have a problem with alcohol. This paper contends that it is equally important to strengthen family support as members of the family assisting the addicted in their recovery process equally require interventions. The paper offers understanding of building coping and resiliency in the individuals and the families Key Words: Alcohol addiction, recovery, de-addiction, individual with an alcohol addiction, family support, strengths based practice; resilience Introduction: Drinking alcohol is as old as civilization. There is hardly any country, community or age in which drinking alcohol did not prevail and there are many cultures where the ingestion of alcohol beverage is regarded as a sign of respectability and modernism (Ghosh, 1999). About 10 to 15% of alcohol users develop alcohol dependence and become alcoholics. Anybody can become an alcoholic - age, education, intelligence or socio-economic status has nothing to do with it. Large amount of revenue is generated from sale of alcohol. Yet, the hidden, cumulative costs of health care, absenteeism and reduced income levels related to heavy alcohol use are higher. These costs were estimated to be 60% more than the revenue generated in a study from Karnataka.The person increases the quantity or frequency and continues drinking even though alcohol causes problems to his health, work life, family or social relationships. Alcoholism is often termed as a “family illness”, referring to its tremendous impact on the family living with an individual with alcohol addiction. The impact of individual with alcohol addiction on socio-economic and psychological wellbeing of the family is obvious enough, which demands urgent intervention. Families living with individual with alcohol addiction interrupt normal family tasks, conflicts in day-to-day living, economical drain of the family resources and leading life with social stigma becomes the characteristic of the family. Children living in the family with alcohol addiction also bound to face many challenges. It is widely accepted that alcohol problems especially in a parent, contributes to the children’s risk and vulnerability. Many studies reveal that children whose biological parents especially the father engaging in substance abuse have a higher risk of developing alcohol problem at an earlier age and male children are found to be more vulnerable with a four-fold risk (Muralidhar & Shankaran, 2007). Alcoholism is treatable. With treatment it is possible to assist the client, however, as with other diseases, the earlier the help is sought, the lesser the damage and the better the recovery. In this paper, we will attempt to write about the need for family interventions and the efficacy of medical psychiatric social work in collateral work with the family. Alcohol Consumption in India Alcohol consumption has been steadily increasing in developing countries like India and decreasing in developed countries since the 1980s. The pattern of drinking to intoxication is prevalent in developing countries indicating higher level of risk due to drinking. Research in the past few years has conclusively demonstrated that nearly one in three male adults consume alcohol, and 5% of Indian women are already regular users. Interestingly, the age of initiation of drinking is progressively coming down. The following inset describes the extent of the problem in India.
The State Response Efforts to address the growing problem of alcohol have been extremely limited in India. It is suggested that this may be due to the large revenue that the consumption of alcohol generates in the country. The prevalence of alcohol into peri-urban, rural and transitional towns and cities, changing lifestyles, liberalized values among youth has figured amongst the clinicians, and in a number of studies (Gururaj, Murthy, Rao, and Benegal, 2011). Non-availability of good-quality data; lack of a central coordinating agency; non recognition of health; social and economic consequences; incorrect interpretation of health benefits and the impact of globalization have all contributed to the problem (Gururaj et.al, 2011). In its recommendations the National Institute of Mental Health and Neuro Sciences ( NIMHANS) report titled ‘Alcohol related harm : Implications for Public Health and Policy in India’ ( 2011) laid emphasis on:
The However, the Nimhans report claims that there is no systematic evaluation with regards to identification of the efficacy and effectiveness of the efforts made which include:
Need for Family Intervention: Less is written, documented and researched on the passive suffers in the family with individual with alcohol addiction especially spouses and children of the individual with alcohol addiction. The families living with individual with alcohol addiction usually hide the alcohol related problem in the family as a shameful secret and thus participate in the dysfunctional behavior. Families experiencing problems with alcohol dependence are fragile, and harm related to alcohol is not confined to the drinkers themselves problem drinker despite alcoholism being characterized as a family illness (Sanikaran, Muralidhar & Benegal, 2008). A number of studies on domestic violence suggest that while alcohol abuse by the spouse may not be the primary cause of domestic violence, it increases a woman’s vulnerability to violence perpetrated by her spouse or partner (Prabhu, Patterson, Dulmus and Ratheeshkumar,2010). Francis (2012) refers to Gerhart (2012) that developed a collaborative appreciative approach of working relationship with the clients and their families cited by Francis, 2012). The collaborative approach of describes the quality of working relationship in which consumers’ voices are respected and valued in the recovery process. The appreciative aspect of model is recognises and values the strengths and abilities of consumers, which generates the necessary momentum for recovery. Some of the practical elements in this approach that are considered very useful are
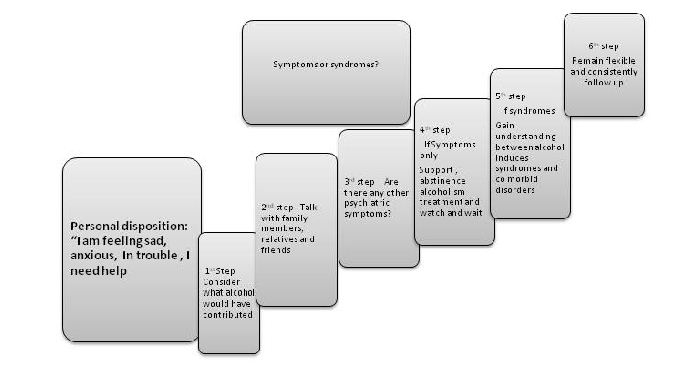
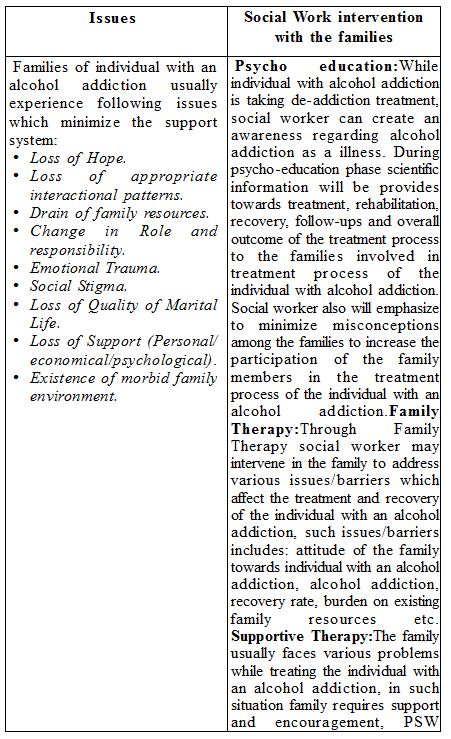
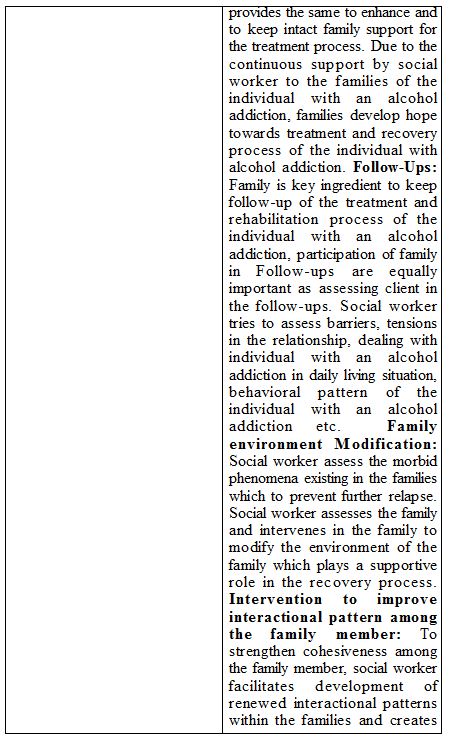
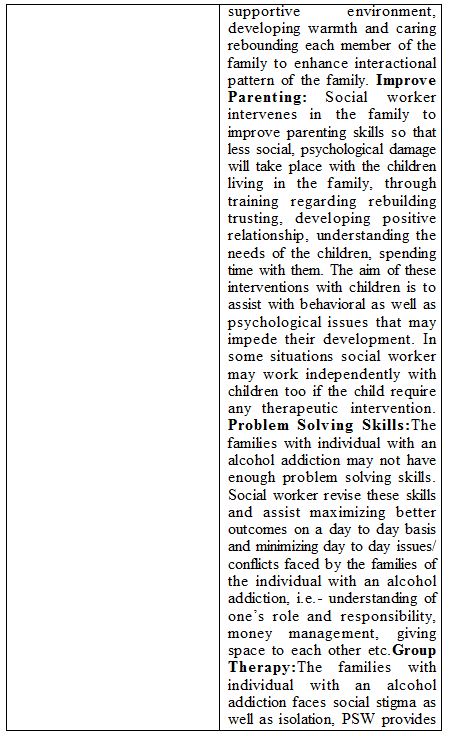
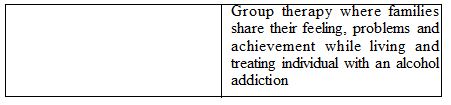
While alcoholism is classifies as a mental health disorder, the evaluation of psychiatric complaints in patients with alcohol use disorders (i.e., alcohol abuse or dependence, collectively called alcoholism) can sometimes be challenging. Heavy drinking associated with alcoholism can coexists with and contributes to a number of several different psychiatric syndromes ( Shivani, 2002). Assessment difficulties It is said that heavy alcohol use directly affects brain function and alters various brain chemical and hormonal systems known to be involved in the development of many common mental disorders (e.g., mood and anxiety disorders). In Medical Psychiatric social work we notice that clients with alcoholism express themselves as being sad and lack in concentration and are fidgety and sometimes they weep. The patient’s symptoms and signs may vary in severity depending upon the amounts of alcohol used, and the longevity of usage. Larger amounts may be associated with more dramatic changes in mood, such as sadness, irritability, and nervousness. Alcohol’s dis-inhibiting properties may also impair judgment and unleash aggressive, antisocial behaviors that may mimic certain externalizing disorders, such as antisocial personality disorder. For instance, an alcohol–dependent patient who appears morbidly depressed when acutely intoxicated may appear anxious and panicky when acutely withdrawing from the drug (Anthenelli 1997). In addition to the direct pharmacological effects of alcohol on brain function, psychosocial stressors that commonly occur in heavy–drinking alcoholic patients (e.g., legal, financial, or interpersonal problems) may indirectly contribute to ongoing alcohol–related symptoms, such as sadness, despair, and anxiety. These above areas are certainly in the realm of social work. Publication of the DSM–IV provided the Psychiatric social workers and clinicians to understand several “alcohol–induced disorders” rather than having to lump alcohol–related conditions under the more generic rubric of an “organic mental syndrome” (Anthenelli 1997). Assessment methodology Clients with alcoholism do not voluntarily disclose information about their alcohol use patterns and problems when they present their psychiatric complaints unless they are asked directly about their alcohol use. They tend to deny and minimize their alcohol–related problems lead them to withhold this important information, which makes assessment and diagnosis difficult. As heavy alcohol use can blur or impair memory, the information given by the patient’s during the history–taking also is less reliable. Therefore, Medical psychiatric social workers should gather information from family sources to make the assessment holistic. After obtaining a patient’s consent his or her history should be obtained from the patient and his family members including spouse, relative, or close friend. The information from family informant interviews yield can serve several purposes. First, by establishing how patterns of alcohol use relate to psychiatric symptoms and their time course, a clinician obtains additional information that can be used in the longitudinal evaluation of the patient’s psychiatric and alcohol problems, as described later. Second, by defining the role alcohol use plays in a patient’s psychiatric complaints, the clinician is starting to confront the patient’s denial, which is the patient’s defense mechanism for avoiding conscious analysis of the association between drinking and other symptoms. Third, by knowing that the clinician will be talking to a family member, the patient may be more likely to offer more accurate information. Fourth, if the patient observes that the clinician is interested enough in the case to contact family members, this may help establish a more trustful therapeutic relationship. Fifth, by involving family members early in the course of treatment, the clinician begins to lay the groundwork toward establishing a supporting network that will become an important part of the patient’s recovery program. Finally, the collateral informant can provide supplemental information about the family history of alcoholism and other psychiatric disorders that can improve diagnostic accuracy (Anthenelli 1997; Anthenelli and Schuckit 1993). A review of the patient’s medical records is another potentially rich source of information. This review should look for evidence of previous psychiatric complaints or of laboratory results that might further implicate alcohol in the patient’s psychiatric problems. Thus assessments carried out collaterally will assist us as social workers in helping the patient and the families through the recovery process in a proper manner. Recovery principles Francis, 2012, complied the following ten key principles of Following is a table consisting of 10 recovery that he adopted from adopted from a previously literature survey conducted by UK by Shepard et.al in 2008, as cited in Francis, ( 2012) 1. Recovery is about building a meaningful and satisfying life, as defined by the person themselves, whether or not there are ongoing or recurring symptoms or problems. 2. Recovery represents a movement away from pathology, illness and symptoms to health, strengths and wellness. 3. Hope is central to recovery and can be enhanced by each person seeing how they can have more active control over their lives (‘agency’) and by seeing how others have found a way forward. 4. Self-management is encouraged and facilitated. The processes of self-management are similar, but what works may be very different for each individual. No ‘one size fits all’. 5. The helping relationship between clinicians and patients moves away from being expert/patient to being ‘coaches’ or ‘partners’ on a journey of discovery. Clinicians are there to be ‘on tap, not on top’. 6. People do not recover in isolation. Recovery is closely associated with social inclusion and being able to take on meaningful and satisfying social roles within local communities, rather than in segregated services. 7. Recovery is about discovering – or re-discovering – a sense of personal identity, separate from illness or disability. 8. The language used and the stories and meanings that are constructed have great significance as mediators of the recovery process. These shared meanings either support a sense of hope and possibility, or invite pessimism and chronicity. 9. The development of recovery-based services emphasizes the personal qualities of staff as much as their formal qualifications. It seeks to cultivate their capacity for hope, creativity, care, compassion, realism and resilience. Family and other supporters are often crucial to recovery and they should be included as partners wherever possible. However, peer support is central for many people in their recovery. (shepherd et al. 2008 cited in Francis, 2012) Strengths Approach The authors believe that a strengths based practice (Pulla, 2012, Pulla and Mariscal, 2013) that has an emphasis on positive qualities and attributes, is quite likely to produce a different approach to social work practice with the families with alcoholic as well as clients that have a problem with alcohol. The methodology as detailed in the strengths perspective clearly assists in helping clients to identify, appreciate, and use their available strengths (Weick et al., 1989). As we move towards the recovery phase it becomes important to identify their talents, knowledge, abilities, and aspirations. During the doctoral research of the first author it was discovered that a number of clients took to alcoholism as a matter of escaping from the ground realities. These realties did include, difficulties and issues with money management, difficulties at work lack of finding work or inability to retain work and or poor wages or inability to simply control as it has become a daily ritual or practice. In raising questions such as ‘what would you be doing if you were not to be drinking?’ provides an opportunity to assist the clients to regain their personal power. This does not happen in the first sitting with the client. It is important questions that will assist clients reclaim their personal power in their lives. The aim is to identify and develop personal and environmental strengths. Dennis Saleebey calls this process the as process that promotes healing and completeness, as individual see in front of them their chances to develop some control over their lives and make decisions than impact them (Saleebey, 1996). When we assume that an individual is the cause of personal pain and social problems (e.g. blaming), we focus on the individuals instead on the social structure. For instance, we may blame a battered woman for staying in an abusive relationship with an alcoholic husband instead of focusing on patriarchal values or the lack of available community resources that might the recovery process and also assist the family to resilience. We believe that strengths based social work approach encourages social workers to use the client’s and families personal strengths and to discover resources in the environments to fulfill the client’s needs and also the family needs to enhance the client’s as well as family’s coping and resilience mechanisms. Thus creation of a helping environment, by itself is an important task of social work. Research in the field of coping suggests that a number of people use emotion-focused coping that rests on denial of the problem. It is not only the individual with the problem of alcohol, but even his family members to an extent may deny the severity of the problem. There is also the tendency to avoid the discussion around their problems despite resulting in poorer overall health and growing including mental health (Pulla, 2013). On the contrary problem focused or action-oriented coping is strongly related to positive psychological outcomes. Although the importance of culture has been recognized, we still do not have well developed constructs that facilitate cross-cultural research with an emphasis in ecology. Strengths based practice suggests that resources are an inherent part of every culture (Pulla, 2012). It is important to address the importance of congruence or the good fit or lack of fit between demands and coping resources that determines the occurrence of stress and the ability of an individual to successfully meet the challenge. Thus, coping and becoming resilient is dependant on the amount of resources available for the individual and the family Pulla, 2013). It is possible to conceive a two step model when the individual recognises the stresses and strains associated with his or her problem, for example the frequency with which he or she is getting into the habit; the costs associated with it. The costs as we suggest would include non monetary costs as well such as the behavioural and mental health issues, personal perceptions of his ore her incidence of drinking etc. If one is cognitively thinking at this step clearly this is a stage where he or she can initiate further steps to mitigate potential stressfulness of the situation. Most often if assistance or help is unavailable at this stage he or she will enter into a secondary coping situation which not actually might be counter productive and increase his intake of alcohol. A number of people with alcoholic condition tend to explain their condition itself as their coping and claim their entrapment to various things around them and absolve their own responsibility. They would even argue with social workers that this is their coping and that they are operating on the principle of ‘what works’ for them in those situations. Certainly in relation to alcoholism, more research in coping and secondary coping is required. The following pathways diagram assists social workers in their work with an individual with alcoholism in his or her recovery and rehabilitation. Pathways diagram based on work of Shivani, Goldsmith and Anthenelli, (2002 ) Suggested Issue based intervention with the families Families of individual with an alcohol addiction usually experience a number of issues such as Loss of Hope; Loss of appropriate interactional patterns, dwindling family resources; difficulties in controlling their emotions and or reacting to traumatized incidents within home. In addition to these, households that have a male member or the head of the household regularly drinking, the family has to bear social stigma. We have outlined some of the issues and attempt here the possible social work interventions. Conclusion:
Capacity building of various stakeholders to carry out prevention and intervention activities with the participation of various stakeholders including the government, nongovernment and community based organizations and education and information dissemination that could create a high degree of public awareness and dissuade harmful alcohol use practices is needed. Families living with individual with alcohol addiction have been considered as passive sufferer and usually do not get attention and intervention in-terms of Bio-Psycho-Social treatment modalities. The paper revealed that families need to have social work intervention to strengthen themselves in the process of treatment and recovery of the individual with alcohol addiction. The study also indicates an urgent need to develop Bio-Psycho-Social intervention plan for the families living with individual with alcohol addiction. The responsibility to develop and deliver the Bio-Psycho-Social intervention for these passive suffers lies with mental health professionals such as Psychiatrist, Clinical Psychologists and especially Social workers. References: 1. Antheneilli, R, M. A basic clinical approach to diagnosis in patients with comorbid psychiatric and substance use disorders. In Shivani, R, Goldsmith, J, Anthenelli, R,M, (2002) ‘Alcoholism and Psychiatric Disorders’ in Alcohol Research and Health, Vol. 26, No.2., http://pubs.niaaa.nih.gov/publications/arh26-2/90-98.pdf retrieved 24/7/2013 2. Antheneilli, R, M.and Schuckit, M, A. Affective and anxiety disorders and alcohol and drug dependence: Diagnosis and treatment, Journal of Addictive Disorders, 12: 73, 1993 cited in Shivani, R, Goldsmith, J, Anthenelli, R,M, (2002) ‘Alcoholism and Psychiatric Disorders’ in Alcohol Research and Health, Vol. 26, No.2., http://pubs.niaaa.nih.gov/publications/arh26-2/90-98.pdf retrieved 24/7/2013 3. Francis, A. (2012) Journey towards recovery in mental health. In V. Pulla, L. Chenoweth, A. Francis & S. Bakaj (eds) Papers in Strengths Based Practice. Dehli, Allied Publishers, pp. 19-33. 4. Ghosh, B (1999) Contemporary Social Problem of India, Himalaya Publishing House, Mumbai 5. Gururaj G, Pratima Murthy, Girish N & Benegal V. (2011) Alcohol related harm: Implications for public health and policy in India, Publication No. 73, NIMHANS, Bangalore, India 6. Indian Alcohol Policy Alliance (2013), ‘Alcohol related Harm In India, a fact Sheet’, by Indian Alcohol Policy Alliance, New Delhi 7. Muralidhar, D & Shankaran, L (2007): Strengths based approach in social work practice in working with families with alcohol problem, Handbook of Psychiatric Social work NIMHANS Publication, first edition Bangalore, Pg- 89-100. 8. Pulla, V., ‘What are Strengths based Practice all about? In Pulla, V., Chenoweth, L., Francis, A., Bakaj, S. eds .,(2012). Papers in Strengths Based Practice, New Delhi: Allied Publishers 9. Pulla, V., Francis A, (2013) A Strengths Approach To Mental Health in Francis,A, (edited) in Social Work practice in Mental health care: Theories, Practices and Challenges. Sage International- (In press) http://www.sagepub.com 10. Pulla, V & Mariscal ,S. (2013). ‘Strength-Based Approach for Social Change’ in Contemporary of Social Work Education, Training and Practice, A, Azman,J, Sulaiman, P Singh J, Singh and M , T Mohamad. ( eds.) KL, Malaysia. Institut Social Malaysia, Ministry of Women, Family and Community Development. ISBN No: 978-967-5472-13-8. 11. Pulla, V, (2013), Contours of Coping and Resilience: the front story in Pulla, V, Shatte, A and Warren , S. eds, (2013) Perspectives on Coping and Resilience, Authors Press, New Delhi 12. Sankaran, L, Muralidhar, D and vivek Benegal. (2008). Strengthening Resilience within Families in Addiction Treatmet. Mumbai: The Indian Journal of Social Work ,Volume- 69, TISS. 13. Sanikaran, Muralidhar & Benegal (2008): Strengthening Resilience within Families in Addiction Treatment, The Indian Journal of Social work, TISS, Vol-69, Issue-I, Pg-45-53. 14. Saleebey, D. (1996). The Strengths Perspective in social work practice: Extensions and cautions. Social Work, 41(3), 296. 15. Shivani, R, Goldsmith, J, Anthenelli, R,M, (2002) ‘Alcoholism and Psychiatric Disorders’ in Alcohol Research and Health, Vol. 26, No.2., http://pubs.niaaa.nih.gov/publications/arh26-2/90-98.pdf retrieved 24/7/2013 16. Shraddha Prabhu, David A. Patterson, Catherine N. Dulmus and Ratheeshkumar K S (2010): Prevalence, Nature, Context and Impact of Alcohol Use in India: Recommendations for Practice and Research, Journal of Global Social Work Practice, Volume 3, Number 2. http://www.globalsocialwork.org/vol3no2/Prabhu.html (Visited on 13/8/12). 17. Weick, A., Rapp, C. A., Sullivan, W. P., & Kisthardt, W. (1989). A Strengths Perspective for Social Work Practice. Social Work, 34(4), 350. Jitendra S. Gandhi Assistant Professor, Department of Social Work, Walchand College of Arts and Science, Solapur, Maharashtra (India) email- [email protected] Venkat Pulla Dr Venkat Pulla teaches Social Work at the Charles Sturt University. [email protected]; [email protected] |
Categories
All
Social Work Learning Academy50,000 HR PROFESSIONALS ARE CONNECTED THROUGH OUR NIRATHANKA HR GROUPS.
YOU CAN ALSO JOIN AND PARTICIPATE IN OUR GROUP DISCUSSIONS. MHR LEARNING ACADEMYGet it on Google Play store
|
SITE MAP
SiteTRAININGJOB |
HR SERVICESOTHER SERVICESnIRATHANKA CITIZENS CONNECT |
NIRATHANKAPOSHOUR OTHER WEBSITESSubscribe |
MHR LEARNING ACADEMY
50,000 HR AND SOCIAL WORK PROFESSIONALS ARE CONNECTED THROUGH OUR NIRATHANKA HR GROUPS.
YOU CAN ALSO JOIN AND PARTICIPATE IN OUR GROUP DISCUSSIONS.
YOU CAN ALSO JOIN AND PARTICIPATE IN OUR GROUP DISCUSSIONS.
|
|





 RSS Feed
RSS Feed





